Viewpoints—Telehealth: A Q&A With Melanie Criss
Melanie Criss, OTD, OTR/L, is the owner of Community Therapy Services in Maumee, Ohio. Her company provides occupational therapy telehealth services to children across the United States who attend online charter schools. Jana Cason, DHSc, OTR/L, FAOTA, a Professor at Spalding University’s Auerbach School of Occupational Therapy, in Louisville, Kentucky, recently interviewed Dr. Criss about how telehealth helps her serve clients.
What population does your telehealth program serve?
We currently work with school-aged children, kindergarten through 12th grade, who attend online charter schools and participate in special education programming. The services are considered to be school-based and are aligned with each child’s individualized educational program (IEP). However, because the children attend school in an online context, often from their homes, therapy services also occur in the children’s homes.
How many occupational therapy practitioners are involved in delivering services in your telehealth program?
The telehealth program began in 2009 with one occupational therapist (OT) and has expanded to include 29 OTs and four occupational therapy assistants who provide services to more than 800 students annually across 21 states.
What type of occupational therapy services do you provide through telehealth?
We provide evaluation and intervention services, both direct and consultative, aligned with the students’ IEPs. Interventions target educationally relevant needs, specifically in the areas of sensory processing, emotional regulation, fine motor, visual motor, visual perception, executive functioning, and independent living skills. Consultation with caregivers is a critical component of intervention sessions to facilitate successful student participation in their online education program.
What technology do you use?
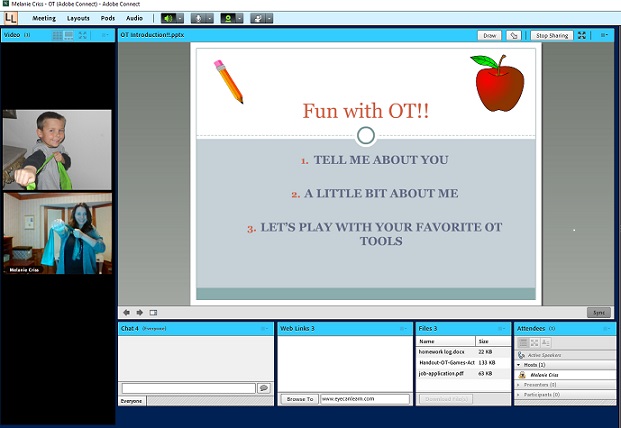
We use Adobe Connect, a subscription-based videoconferencing platform. This is the same platform that many of our schools use for their online classes, so it is familiar to the students. Practitioners use a computer (desktop or laptop) coupled with an external webcam to allow for various degrees of movement and an improved visual field as compared with a built-in web camera. All students have access to a laptop or desktop computer and an external web camera.
How are services provided through your telehealth program paid for/reimbursed?
We contract with school systems and individual schools. Services are paid for through these contracts.
Why did you begin providing services through telehealth?
We began providing occupational therapy services through telehealth in 2009 because of an identified need in primary and secondary online schools. They were having difficulty locating related service providers who could provide services outlined in the students’ IEPs because the children were scattered over large geographic regions due to the nature of online schools. It was not uncommon to have delays in service delivery because the schools had difficulty locating service providers for the students. By delivering services through telehealth, students are able to receive the services identified on their IEP without delay, regardless of location. Additionally, as a related service provider whose primary role is to support students in their educational environment, telehealth enables us to work with the children in their natural school environments, which are also online.
What benefits have you observed from using telehealth?
We have observed numerous benefits to using telehealth in the online school-based setting, including increased access to OTs and their services. Telehealth transcends geographic limitations and provides an opportunity to match a student’s needs with practitioners’ areas of expertise. With telehealth use, there can be increased educational opportunities for caregivers and teachers; decreased need for travel (with both cost and time savings); decreased health risks for students with compromised immune systems; and for some students, increased attention and decreased behavioral challenges when using a technology platform for intervention.
What challenges have you encountered?
Technical difficulties present the greatest challenges we have experienced with telehealth use. Although access to technology can provide far more benefits than challenges, some clients do not have adequate Internet speed to support videoconferencing, and some clients have difficulty understanding the technology tools. However, more often than not, the students and caregivers are very comfortable with the technology and, on occasion, teach the practitioners strategies for increased ease of use. Another challenge is lack of license portability and the time and cost associated with obtaining and maintaining multiple state occupational therapy licenses. A majority of our OTs maintain three or more state occupational therapy licenses, and one OT maintains 17 state licenses to serve children from many diverse geographic areas.
What recommendations or “lessons learned” would you like to share with other practitioners interested in telehealth?
First, despite impressive technological advancements, technological difficulties are inevitable, and you will experience them at some point. Having a plan in place for when technology fails can decrease the level of stress in those moments. Second, effective communication with the caregivers is essential to achieving student follow-through with your recommendations throughout the week. Developing rapport with the student and caregiver early on and discussing expectations are essential parts of a successful intervention plan in the telehealth environment.
Do you have any other thoughts you would like to share?
It is critical to consider the ethical implications associated with using telehealth. Telehealth services should not be a blanket approach for all clients, but rather, decisions for client appropriateness should be individualized and determined case by case. Clients need to be fully informed of the benefits and challenges associated with telehealth and be given the right to refuse telehealth intervention. Practitioners should be familiar with the American Occupational Therapy Association’s Occupational Therapy Code of Ethics and Ethics Standards; laws and regulations associated with confidentiality; and state licensure, supervision, and telehealth laws and regulations for both the state they reside in as well as the state in which each client resides.
Jana Cason, DHSc, OTR/L, FAOTA, is a Professor at Spalding University’s Auerbach School of Occupational Therapy, in Louisville, Kentucky. Explore AOTA resources on telehealth. To be considered for inclusion in a future telehealth Q&A, email jcason@spalding.edu.