Helping to Develop a Gaming Device
As technology evolves, rehabilitation gaming devices are becoming more sophisticated at meeting client rehabilitation needs—with the potential to improve performance skills such as range of motion, coordination, and strength and to perform ADLs. Gaming devices can be motivating because of their visual interface and their ability to allow clients to track their progress. Gaming devices can be portable enough to take home, enabling carryover of therapeutic interventions (Saposnik et al., 2010).
Although new rehab gaming devices are continually being developed, determining which are most useful to your patient population can be difficult because evidence comparing them with traditional therapy interventions is insufficient (Hijmans et al., 2011; Thomson et al., 2014; Verbeek et al., 2014). Additionally, some devices are developed without input from rehabilitation professionals early in the process, so the device components do not meet client needs and are not adopted into practice.
Occupational therapists (OTs) have skills that are invaluable to developers who are bringing rehab gaming devices to market. When compared to other rehabilitation team members, OTs have unique frameworks to understand how a device might help with the client’s performance skills that influence participation in daily occupations. In addition, occupational therapists have extensive knowledge about vision and cognition and how these systems might influence the ability for clients to use such devices.
Developers and designers need therapy professionals to test, research, and market products designed for the rehab market to enhance the clinical adoption. Designers must solicit feedback from not only patients, but also from therapists because therapists understand how clients with different conditions will actually use and potentially benefit from the device.
In the winter of 2018, I was approached by Ashesh Patel, Founder and CEO of Ashana Health, who is orchestrating the development of the Dynawheel, a device for individuals with upper-extremity limitations. The games on the device include a racing game, a “basket catch” game, and a maze. Each game targets different performance skills and can be adjusted for the patient.
Ashesh said he was inspired to develop the Dynawheel after observing his grandfather participate in therapy after having a stroke. He noted, “I was watching the patients and noticed that there was not much to motivate them to participate. I decided that I wanted to work on something that would help motivate them.”
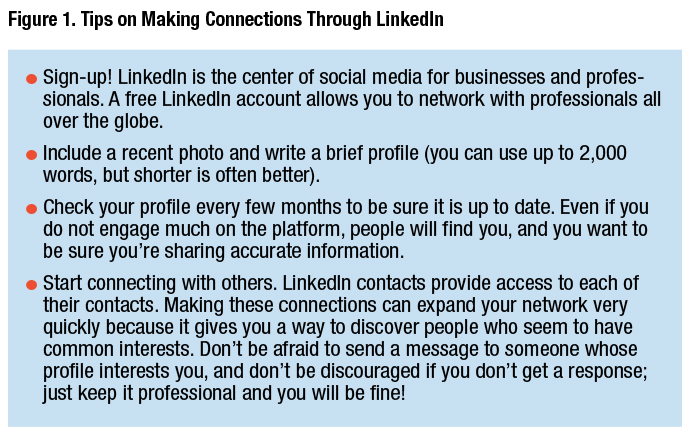
Ashesh contacted me through LinkedIn (see Figure 1 for tips on making sure you are set up to network), asking if I would be interested in testing the Dynawheel and providing feedback on its usability.
I thought he had a great idea and passion for the product and was happy to help. Although the device is fairly simple, it had some key features that interested me:
- It’s lightweight and portable so clients could use it anywhere;
- The bilateral handles need to be squeezed during key points in the games, addressing grip strength;
- It must be tilted to move objects on the screen, addressing range of motion;
- Users must track objects, addressing visual motor coordination;
- It automatically tracks client progress; and
- It includes different types of games to address various client interests.
We conversed over the course of a few months and met at the American Occupational Therapy Association Annual Conference & Expo, where I was able to play with the Dynawheel for the first time (see Figure 2). Although it was just a prototype, I thought it had potential, and I shared with Ashesh how it might be adapted to be more relevant to occupational therapists and clients. Ashesh wanted data to support use of the device, and I agreed to gather therapist feedback and develop a clinical study on the motivation and function of clients using the device.

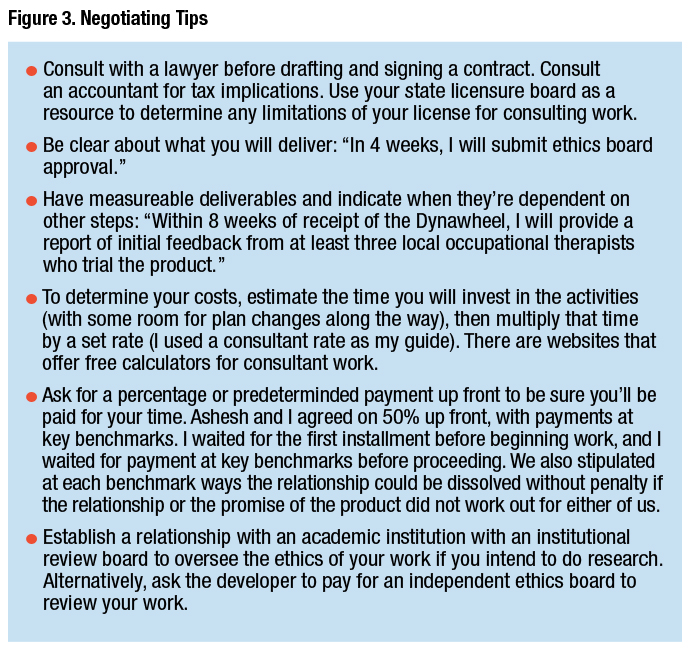
After some discussion, Ashesh and I decided on the details of a contract. Ashesh would pay me as a consultant to solicit feedback from occupational therapists, develop a small research study with the product, and write articles to help spread the word about the Dynawheel. Because I had not made this kind of arrangement before, I drafted goals for the relationship and provided a price estimate. He replied with what he wanted me to do and some other items that he felt his team would be able to complete, and also proposed some changes to some of the contracted prices. We were able to come to an agreement to proceed with the work (see Figure 3 on for negotiating tips).
After we had signed the contract, Ashesh sent me a prototype and I went to work. I approached former colleagues and willing therapists to provide feedback, and I shared my own based on my experience in occupational therapy.
Meanwhile, I developed the protocol for a small exploratory study for a group of older adults using the device and submitted the institutional review board documents to my university. I hired a research assistant to help with data collection (which was negotiated in the contract). The study included collecting information about occupational performance and performance skills (particularly range of motion and strength) of the upper extremity, and motivation for current therapeutic activity and while using the device.
The preliminary feedback I provided to Ashesh was used to update the device, notably with a larger adjustable screen and a more streamlined design to improve portability (see Figure 4).

Exploratory Study
The original study was unfortunately cut short amid concerns over the novel coronavirus. In the previous 4 months, we had interest from 10 clients at a local facility where one of the therapists who provided initial feedback on the device worked. Participants were enrolled after they signed an informed consent outlining the risks and benefits and allowing the results to be shared. The clients used the device and gave feedback on how they liked it.
We originally enrolled seven participants across two sites; they were already in rehabilitation programs supervised by an occupational therapist. We conducted an initial occupational therapy evaluation that included a version of the Intrinsic Motivation Inventory (McAuley et al., 1989; Pelletier et al., 1997) to measure motivation with therapeutic activities before and after use of the Dynawheel. At baseline, we analyzed users’ motivation for typical therapy activities; at subsequent sessions, we measured their motivation for using the Dynawheel. We also used the Disability of the Shoulder, Arm, and Hand questionnaire (Gummesson et al., 2003) to collect information on clients’ functional abilities.
From initial use of the Dynawheel to the 6-week data collection point, participants’ motivation for participating in therapeutic activities, including using the Dynawheel, had increased. However, one of the participants stated, “I was never a video game player so it was hard for me to get used to,” highlighting the need for meaningful activities in occupational therapy interventions. Another participant needed one-on-one help to correctly use the device. Overall, the participants said they were happy to have the opportunity to do something new and different in their therapy sessions.
Future Directions
Since the changes that have been imposed by the pandemic, I have been exploring how the Dynawheel could be used in and out of the clinic. For example, for patients whose compliance decreases with teletherapy, a gaming device like the Dynawheel might increase motivation to participate in therapeutic activity without a therapist present. We are continuing to look at options for moving forward. I believe that occupational therapists have a lot to offer research and development teams who are developing gaming devices, but these teams might not understand the value of the input of an occupational therapist. Occupational therapists should feel confident approaching developers and explaining our distinct value. The added value of having an OT on a team can be crucial to understanding how the device might be used by a client and how using the device might improve daily living skills. This will ultimately lead to wider adoption of the device because it has been thoughtfully developed with usability and functional outcomes in mind.
References
Gummesson, C., Atroshi, I., & Ekdahl, C. (2003). The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: Longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskeletal Disorders, 4, 11. https://doi.org/10.1186/1471-2474-4-11
Hijmans, J. M., Hale, L. A., Satherley, J. A., McMillan, N. J., & King, M. J. (2011). Bilateral upper-limb rehabilitation after stroke using a movement-based game controller. Journal of Rehabilitation Research & Development, 48(8), 1005–1013. https://doi.org/10.1682/jrrd.2010.06.0109
McAuley, E., Duncan, T., & Tammen, V. V. (1989). Psychometric properties of the Intrinsic Motivation Inventory in a competitive sport setting: A confirmatory factor analysis. Research Quarterly for Exercise and Sport, 60(1), 48–58. https://doi.org/10.1080/02701367.1989.10607413
Pelletier, L. G., Tuson, K. M., & Haddad, N. K. (1997). Client Motivation for Therapy Scale: A measure of intrinsic motivation, extrinsic motivation, and amotivation for therapy. Journal of Personality Assessment, 68(2), 414–435. https://doi.org/10.1207/s15327752jpa6802_11
Saposnik, G., Teasell R., Mamdani M., Hall J., McIlroy W., Cheung D., … Bayley, M.(2010). Effectiveness of virtual reality using Wii gaming technology in stroke rehabilitation: A pilot randomized clinical trial and proof of principle. Stroke, 41, 1477–1484. https://doi.org/10.1161/STROKEAHA.110.584979
Thomson, K. K., Pollock, A., Bugge, C., & Brady, M. (2014). Commercial gaming devices for stroke upper limb rehabilitation: A systematic review. International Journal of Stroke, 9, 479–488. https://doi.org/10.1111/ijs.12263
Verbeek J. M., Wegen E., Peppen R., Wees P. J., Hendriks, E., … Rietberg, M. (2014). What is the evidence for physical therapy poststroke? A systematic review and meta‐analysis. PLoS One, 9(2), e87987. https://doi.org/10.1371/journal.pone.0087987
Karen M. Keptner, PhD, OTR/L, has had a variety of clinical experience over her 20-plus years as an OT, including in outpatient therapy, acute care and rehab in a hospital setting, home health, school system practice, and skilled nursing, along with community-based practice. She is currently an Associate Professor in the Occupational Therapy program at Cleveland State University in Ohio and primarily does research while looking for new opportunities to innovate and challenge herself in practice.